TL;DR: A pathology report is a detailed medical document written by a pathologist—a doctor who specializes in diagnosing disease by examining tissue. This report is the definitive story told by a tissue sample, providing critical information for medical treatment or legal clarity after a loss. It’s a complex document, but understanding its key sections and terminology can empower you to have more informed conversations with your medical team or legal counsel.
- What it is: A pathology report is the formal conclusion of a pathologist's examination of a tissue sample (biopsy) or a postmortem examination (autopsy).
- Why it matters: It provides the foundational diagnosis for diseases like cancer, guiding treatment decisions. In forensic cases, it establishes the cause of death, offering answers to families and evidence for the justice system.
- Key Sections: Reports are typically structured with Patient Information, a Gross Description (what the tissue looks like), a Microscopic Description (what the cells look like), and a Final Diagnosis (the conclusion).
- Essential Terms: Knowing the difference between terms like benign (non-cancerous) and malignant (cancerous) is crucial for understanding the pathology report meaning.
A Guide to Navigating Your Pathology Report
Receiving a pathology report often comes during a period of great stress and uncertainty. You might be a patient awaiting a diagnosis or a family member seeking answers after the loss of a loved one. The clinical, technical language inside these documents can feel impersonal and overwhelming.
My goal is to demystify this document for you. As a forensic pathologist, I work with these reports daily, and I understand the weight they carry. This guide will walk you through the meaning of a pathology report, step-by-step, so you can feel empowered by its contents, not intimidated.
What We Will Cover Together
Think of this as a road map. We will start with the fundamental purpose of the report and move through its structure, just as a pathologist assembles individual findings to arrive at a conclusion.
Here’s what we'll explore:
- Key Sections: We will break down each part of the report, from patient information to the final diagnostic summary.
- Common Terminology: I will translate some of the most common medical terms into plain language so you can grasp what the findings truly mean.
- The Pathologist's Role: You'll gain insight into the meticulous work behind every analysis. We carry a profound responsibility with each case. If you're interested in the medico-legal side of this discipline, our article on what forensic pathology is offers a deeper look.
- Contextualizing Results: We'll discuss how a report's findings fit into the larger picture, whether for medical treatment or legal proceedings, to clarify what comes next.
By the end of this guide, you should have a solid framework for interpreting a pathology report. It is far more than just data; it is a vital tool for health, closure, and, in some cases, justice.
What Is a Pathology Report? And Why Does It Matter?
A pathology report is the final, definitive story a piece of tissue has to tell. It is a formal medical document authored by a pathologist—a physician specializing in the study of tissues and fluids to diagnose disease. After a sample is examined, this report presents the authoritative conclusion of those findings. It is the bedrock upon which life-altering decisions are built.
When a patient undergoes a biopsy, the pathology report guides their entire treatment plan. It answers the critical questions: Is this growth cancerous? If so, what specific type is it? What are its unique characteristics? This detailed information allows oncologists and surgeons to map out the most effective, personalized course of action.
In my field of forensic pathology, the report serves an equally critical, though different, purpose. Following a postmortem examination (autopsy), it provides clear, medically sound answers to grieving families about why their loved one died. It also becomes a crucial piece of evidence in legal cases, ensuring that justice is firmly rooted in scientific fact.
The Foundation of Medical and Legal Truth
The importance of a pathology report cannot be overstated. It is the document that translates what a pathologist observes through a microscope into actionable knowledge. The process is painstaking, beginning with a careful examination of the tissue with the naked eye (the gross description) before proceeding to high-power magnification (the microscopic description).
A pathology report is far more than a summary of findings. It is the culmination of a rigorous scientific investigation designed to deliver an objective, evidence-based conclusion that can withstand both medical and legal scrutiny.
This report bridges the gap between science and its human impact. For a patient, it can mean the difference between aggressive chemotherapy and a "watch and wait" approach. For a family seeking answers after a death, it can bring closure or provide the grounds needed for legal action.
In moments of profound uncertainty, this document provides a point of certainty. The reliance on this diagnostic work is reflected in its growth; the global pathology services market was valued at USD 18.8 billion in 2025 and is projected to nearly double by 2035. You can explore more on the growth of pathology services here.
Two Main Types of Reports
While the underlying science is the same, the context for the examination shapes its focus. To truly understand the pathology report meaning, it helps to know its origin. There are two primary contexts:
- Surgical Pathology: This involves examining tissues removed from a living person during a procedure, such as a biopsy or tumor removal. The primary goal is to diagnose disease and guide treatment.
- Autopsy Pathology: This involves the examination of a body after death to determine the cause, manner, and mechanism of death. Its purpose is to provide answers for families and objective evidence for the justice system.
Ultimately, both report types are built on a foundation of meticulous observation and precise documentation. They are the final, expert record, delivering clarity when it is needed most.
How to Read Your Pathology Report Section by Section
Receiving a pathology report can feel like being handed a complex legal document, filled with intimidating medical terms and data. However, every report follows a logical pattern. My goal here is to walk you through it, section by section, starting with the basics and working toward the final conclusion, so you can see how each part contributes to the complete story.
The report is designed to flow from general information to the most detailed findings. It starts with the "who" and "what," moves to what the pathologist observes with the naked eye, and then dives deep into the microscopic, cellular level.
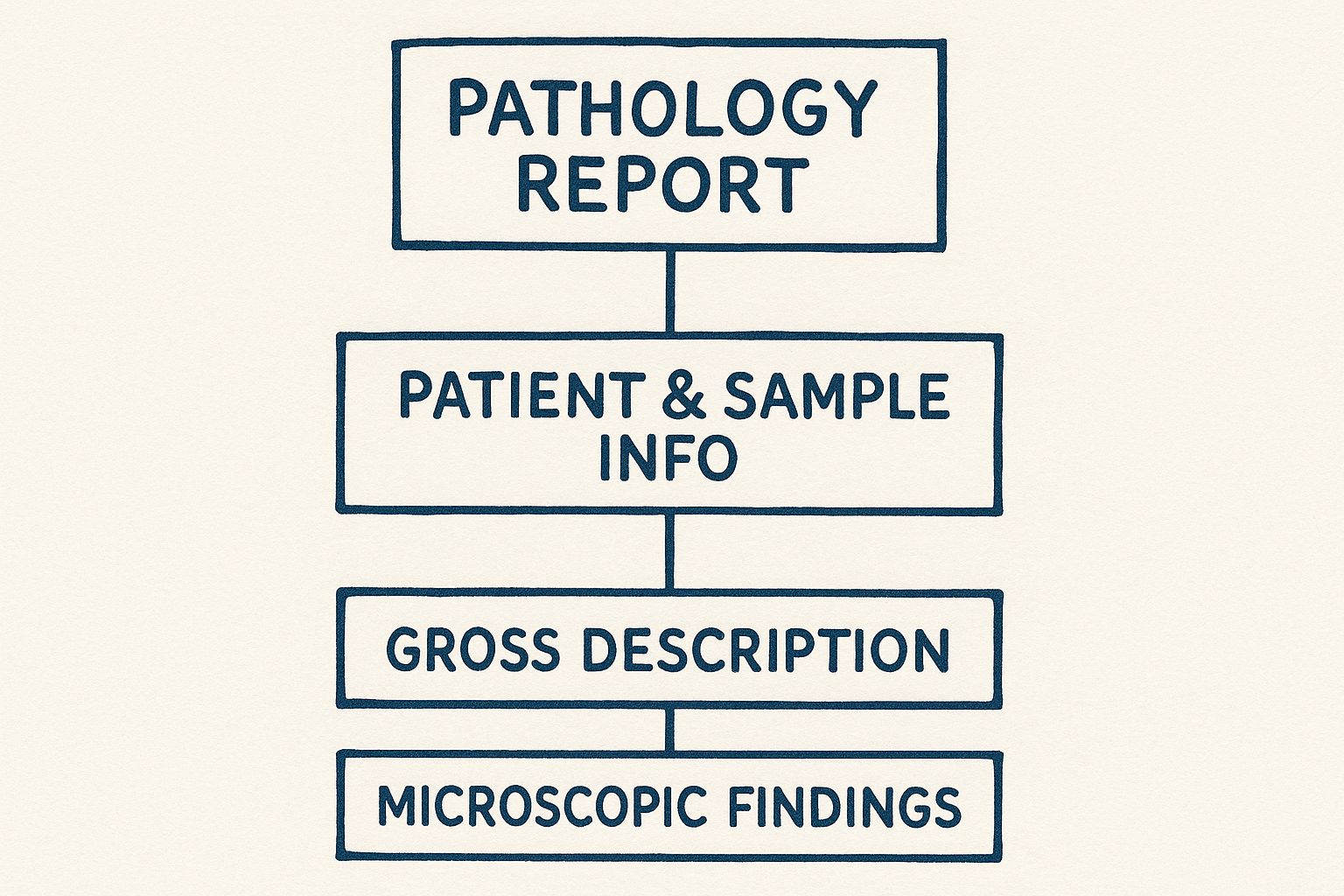
This structure is deliberate. Each section builds upon the one before it, creating a comprehensive picture of the diagnosis. Let’s break down the standard sections you will find in nearly any pathology report.
Anatomy of a Pathology Report
Every report is organized into key sections, each serving a specific purpose. The table below offers a quick overview of what each part is and what it means in simple terms.
| Report Section | What It Tells You |
|---|---|
| Patient Information | Confirms the report belongs to the right person and the right tissue sample. |
| Gross Description | Describes what the tissue looks like to the naked eye—size, color, and shape. |
| Microscopic Description | Details what the pathologist sees under the microscope at a cellular level. |
| Final Diagnosis | The ultimate conclusion—the "bottom line" of the report. |
Now, let's take a closer look at what goes into each of these sections.
Patient and Specimen Information
At the top of the report, you will find administrative details. This may seem like simple paperwork, but it is arguably the most critical part of the entire document. It is the anchor connecting all scientific findings to the correct person and tissue sample.
Here’s what you’ll see:
- Patient Details: The patient’s full name, date of birth, and medical record number.
- Submitting Physician: The doctor who requested the analysis.
- Specimen Details: A unique ID number for the tissue sample, the date it was collected, and where it came from (e.g., "skin biopsy, right forearm").
Ensuring this information is 100% correct is non-negotiable. It is the first and most vital step in preventing mix-ups.
The Gross Description
The next section is the Gross Description. The term "gross" here refers to what is visible to the naked eye, not something unpleasant. This is the pathologist’s first examination of the tissue sample before it is processed for microscopic review. It is akin to a detective describing a scene before dusting for fingerprints.
The pathologist notes the sample's physical characteristics—its size, weight, color, and texture. For a tiny biopsy, this might be a simple note about its dimensions. For a larger specimen, like a removed organ, the description will be far more detailed. This provides essential context for what the pathologist will find later.
The Microscopic Description
This is the heart of the report. Here, the pathologist has taken the tissue, sliced it into paper-thin sections, stained it with special dyes to highlight different cellular structures, and examined it under a high-powered microscope.
This section is technical. It uses precise language to describe how cells are arranged, what they look like, and whether they appear normal or abnormal. It is here that the pathologist pieces together the clues that lead to a diagnosis. To get a better feel for this, you might look at an example pathology report on our blog.
The microscopic description is where the story truly comes to light. It’s a journey into the cellular world, where the definitive evidence of a condition—or its absence—is found.
The Final Diagnosis or Summary
After all examination and analysis, everything culminates in the Final Diagnosis. This is the single most important section of the report. It is the conclusion, stated as clearly and directly as possible.
This section answers the central questions: Is it cancer? Is it benign? What is the specific type of disease? If a tumor was removed, the report will also comment on the margins—the tissue surrounding the tumor—to determine if all cancerous cells were successfully excised. For families and physicians, this is the bottom line.
Decoding Common Medical Terms in Your Report
The highly specialized language in a pathology report can be a significant source of anxiety. My goal here is not to provide a comprehensive medical dictionary, but rather to translate the clinical jargon into clear, understandable concepts. Think of this as a primer to help you have more informed conversations with a medical team or legal counsel.

Understanding these terms can bring immense relief and clarity. A pathology report is an incredibly precise document where every word is chosen for a specific reason. Let’s break down some of the most common—and often most confusing—terms you are likely to encounter.
Foundational Concepts in Pathology
Before diving into specific diagnoses, it helps to understand a few core ideas pathologists use to classify what they observe under the microscope. These terms are the basic building blocks of any diagnosis.
- Neoplasm: This is a general term for an abnormal growth of cells. It is a starting point; the pathologist’s job is to determine if this growth is harmless or something more serious.
- Lesion: Another broad term, a lesion refers to any area of tissue that appears abnormal. It could be from an injury, a disease, or a growth. It simply flags a spot that requires the pathologist's close attention.
- Dysplasia: This word describes cells that look abnormal under the microscope but are not yet cancerous. It is often graded as "low-grade" or "high-grade," indicating how unusual the cells appear. High-grade dysplasia is monitored more closely because it carries a greater risk of progressing to cancer.
Benign vs. Malignant: The Critical Distinction
This is perhaps the single most important distinction in a pathology report. The difference between these two words changes everything.
The core difference lies in behavior. Benign growths are typically localized and do not spread, while malignant growths are invasive and can spread to other parts of the body.
Benign means non-cancerous. A benign tumor may grow larger, but it remains contained—it will not invade nearby tissues or spread to distant parts of the body. It is usually not life-threatening, though its location can sometimes cause issues depending on what it presses against.
Malignant means it is cancerous. These cells are different. They have the ability to invade surrounding tissues and metastasize—the medical term for spreading to other organs via the bloodstream or lymphatic system. This invasive potential is what makes cancer so dangerous.
Key Terms in Cancer Reports
If a report confirms a malignancy, you will encounter more specific terms used to describe its characteristics. Understanding these will give you a clearer picture of the diagnosis.
- Carcinoma: This is the most common type of cancer. It begins in epithelial cells, which are the cells that line the inside and outside surfaces of the body, such as the skin or the lining of organs.
- Invasive/Infiltrating: If you see these words, it means the cancer cells have broken through the original tissue layer where they started. This is a critical factor in determining the cancer's stage.
- Margins: When a surgeon removes a tumor, the pathologist carefully examines the edges of the excised tissue. Negative margins (or “clear margins”) is the good news you hope for; it means no cancer cells were found at the edge, suggesting the entire tumor was removed. Positive margins mean cancer cells are present at the edge, which may indicate that further treatment is necessary.
- Differentiation: This term describes how much the cancer cells resemble normal, healthy cells. Well-differentiated cancer cells look more like normal cells and typically grow more slowly. Poorly-differentiated cells appear very abnormal and tend to be more aggressive, growing and spreading faster.
The language in a report is precise for a reason, but it should not be a barrier to your understanding. These definitions, along with details from other specialized tests like a toxicology report example, are tools to help you find the answers you need.
How Technology Is Shaping Modern Pathology
Pathology has long been a discipline of glass slides and microscopes, but a significant shift is underway. Powerful new technologies are fundamentally changing how we work, leading to faster, more accurate diagnoses and enhancing our ability to provide definitive answers. At the heart of this evolution is digital pathology.
Digital pathology is the practice of converting traditional glass slides into high-resolution digital images, much like scanning an old photograph. Once a slide is digitized, we can view it on a screen, archive it securely, and instantly share it with experts anywhere in the world for a second opinion or specialized consultation.
The Rise of Digital Tools and AI
This digital transition is having a profound impact. The global digital pathology market is expanding rapidly, driven by the need for greater efficiency in diagnostic work. Analysts predict the market could grow from approximately $9.1 billion in 2025 to over $31 billion by 2035. You can learn more about the growth drivers in digital pathology from those who follow the industry.
This is not just about converting slides to pixels; we are now integrating artificial intelligence (AI) into the process. In modern pathology, AI image analysis is becoming an essential tool, helping us interpret incredibly complex visual data with greater accuracy and speed.
AI algorithms can be trained to spot subtle patterns in tissue that might be nearly impossible for the human eye to discern. This technology does not replace the pathologist. Instead, think of it as a highly advanced new tool in our toolkit—one that enhances our own expertise and improves diagnostic precision.
For example, an AI tool can help count tumor cells, identify specific genetic mutations based on cellular appearance, or automatically flag a tiny area on a digital slide that requires closer examination.
These advancements are not merely about speed. They are paving the way for a more personalized approach to medicine, where a diagnosis is directly linked to the unique molecular fingerprint of a disease. By combining digital imaging with AI-powered analytics, the pathology report meaning becomes richer and more detailed, offering insights that guide better treatment and provide clearer answers for families.
The report you hold is a foundational component of both our healthcare and justice systems. Every day, crucial medical decisions and life-altering legal outcomes depend on a pathologist's findings. It is a weight my colleagues and I feel with every case we handle.
The work we do in the laboratory has a direct and real impact on people's lives. A routine screening can catch cancer early enough for effective treatment; a complex forensic investigation can finally bring a family a measure of closure. At its heart, pathology is about finding the truth, one microscopic slide at a time.
A Pillar of Modern Medicine
Pathology is the engine of modern diagnostics. The sheer scale of this field is immense—the global market for pathology labs was valued at around USD 386 billion in 2024 and continues to grow. That figure represents the infrastructure behind millions of reports generated each year, each one playing a critical role in patient care. The analysis from Grand View Research offers a fascinating look at the industry numbers.
More Than Just a Diagnosis
For a patient, a pathology report is the map that guides their entire treatment journey. For a family struggling with loss, it can offer the solid answers needed to begin the grieving process. And in a courtroom, it is often the unshakable evidence that ensures justice is served.
A pathology report is the final word in a careful scientific investigation. It provides an objective, evidence-based foundation that allows doctors to heal, families to find peace, and our legal system to function with integrity.
Your report is not just another piece of paper; it is a critical piece of a much larger story. It is the result of a scientific discipline dedicated to getting things right—whether that means examining a small biopsy from a clinic or conducting a complex postmortem examination.
Frequently Asked Questions About Pathology Reports
After reviewing a report, it is completely normal to have more questions. I have found that families and professionals often wonder about the same practical matters: how long it takes, if the results are certain, and what to do next. Let's address some of the most common questions I receive.
How Long Does It Take to Get a Report Back?
This is perhaps the most common question, and the answer is: it depends. A simple skin biopsy might be resulted in just a couple of days. However, more complex situations, such as a full autopsy or a specimen requiring genetic testing, could take several weeks.
A few factors can affect the timeline:
- Complexity of the Case: A small, straightforward tissue sample is processed much faster than a large tumor requiring examination of many different sections.
- Need for Special Tests: Sometimes, the initial microscopic examination does not tell the whole story. The pathologist may need to order special stains or molecular tests for a precise diagnosis, which adds time.
- Second Opinions: In challenging cases, it is common for a pathologist to consult a colleague. This is a standard part of the quality assurance process to ensure accuracy.
Can a Diagnosis Be Wrong?
Pathologists are meticulous, but since medicine is both a science and an art, errors can happen, though they are rare. The field is built on a foundation of checks and balances to catch potential mistakes. Cases are often reviewed by other pathologists, and findings are always correlated with the patient's clinical symptoms and other test results.
If there is any uncertainty, requesting a second opinion is a standard part of medical care. Having another set of expert eyes review the slides and the report is never a bad idea. This can provide crucial confirmation and, just as importantly, peace of mind.
Who Should I Talk to About My Report?
The best person to discuss your report with is the doctor who ordered it—whether that is your surgeon, oncologist, or primary care physician. They can place the pathologist's findings into the context of your specific health situation.
It is also helpful to understand the difference between a surgical pathology report from a biopsy and a full autopsy report. A pathologist prepares both, but an autopsy report is a far more comprehensive document. It is designed to determine the cause and manner of death and involves a detailed examination of the entire body, both externally and internally.
If you require assistance in understanding a postmortem report or have questions regarding private autopsy services, our team is here to provide clear, compassionate guidance. Please feel free to contact us for more information.

