When a death occurs, the questions can be overwhelming. As a forensic pathologist, I see a toxicology report after death as one of the most powerful tools available to provide clear, scientific answers. It offers a precise biochemical snapshot of what was in a person’s system when they passed away, identifying drugs, alcohol, and other substances. Often, this information is the key to determining the true cause and manner of death, offering clarity during a time of profound uncertainty.
- A toxicology report identifies substances in the body after death.
- It determines if substances caused, contributed to, or were incidental to the death.
- The process involves collecting biological samples during an autopsy, followed by detailed laboratory analysis.
- Interpretation requires expertise to distinguish between therapeutic, toxic, and lethal levels, considering factors like tolerance and postmortem changes.
- These reports are vital for families seeking answers and for legal and insurance matters.
The Critical Role of Postmortem Toxicology
In my work, postmortem toxicology is fundamental to reconstructing a person’s final hours from a biochemical perspective. This analysis is not merely a search for illicit drugs; it’s about assembling a complete picture so families and legal professionals can understand what role, if any, various compounds played in the death.
This scientific investigation is a crucial component of a complete forensic autopsy, capable of revealing evidence that a physical examination alone cannot. If you would like to understand the entire procedure, our guide on what is a forensic autopsy provides a comprehensive overview.
Uncovering Objective Truths
At its heart, a postmortem toxicology report identifies and quantifies substances to help answer vital questions:
- Was a substance a direct cause of death? A lethal overdose of an opioid is a clear example.
- Did a substance contribute to the death? This might involve an individual with heart disease who used a stimulant, or someone whose judgment was impaired by alcohol, leading to a fatal accident.
- Was a substance incidental? For example, a therapeutic level of a prescribed antidepressant would likely be an incidental finding unrelated to the cause of death.
More Than Just Illicit Drugs
A common misconception is that toxicology is only about finding illegal drugs. In reality, a standard toxicology screen is incredibly broad and evaluates a wide range of substances.
A typical analysis will include:
- Prescription Medications: Antidepressants, pain relievers, cardiac medications, and sleep aids.
- Over-the-Counter Drugs: Common substances like acetaminophen or antihistamines, which can be toxic in very high doses.
- Alcohols: This includes ethanol and other volatile compounds.
- Environmental Toxins: If circumstances suggest exposure, we can test for substances like carbon monoxide or heavy metals.
The need for this detailed analysis has never been more pressing. The global overdose crisis continues to escalate, driven largely by powerful synthetic opioids. Here in the United States, the Centers for Disease Control and Prevention reported over 107,000 overdose deaths in 2023, a staggering number that underscores the vital role of precise toxicological testing.
Ultimately, the toxicology report provides impartial, scientific data. For grieving families, it offers definitive answers and helps clarify medical histories. For the legal system, it ensures that insurance and judicial matters are resolved based on fact, not speculation.
How We Collect and Analyze Toxicology Samples
The path from an autopsy to a final toxicology report is a meticulous, step-by-step process. It begins during the postmortem examination itself, where I collect the biological samples that will tell the story of the substances present in the body and in what concentrations.
Each sample is a piece of evidence, offering a unique window into the decedent's final hours. Selecting the right combination of specimens is the first critical step toward building an accurate and complete biochemical picture.
The Art and Science of Sample Collection
During an autopsy, a comprehensive collection of samples is essential, as different fluids and tissues reveal different parts of the story. Some provide a snapshot in time, while others can indicate a longer history of substance use.
The table below outlines some of the most common samples collected and explains their value to the forensic investigation.
Common Samples Used in Postmortem Toxicology
| Sample Type | Primary Purpose | Information Provided |
|---|---|---|
| Blood | To determine what substances were actively circulating in the body at or near the time of death. | This is the most critical sample for assessing impairment and acute toxicity. Peripheral blood (from the femoral vein in the leg) is preferred to avoid falsely high readings caused by postmortem redistribution. |
| Vitreous Humor | To provide a clean, stable sample that resists post-death decomposition and contamination. | The fluid from the eye is excellent for detecting alcohol and certain drugs. Its protected environment often yields a more reliable result than samples susceptible to bacterial changes. |
| Urine | To identify recent drug use, typically within the past few days. | Urine can show evidence of a substance long after it has cleared from the blood, making it ideal for detecting a history of recent use. |
| Liver Tissue | To reveal chronic substance use and identify drugs that have been broken down (metabolized) by the body. | As the body’s primary site for drug metabolism, a liver sample can show what was being processed hours or even days before death. |
Each sample plays a specific role. Together, they allow a pathologist to cross-reference findings and build a much stronger, more reliable conclusion.
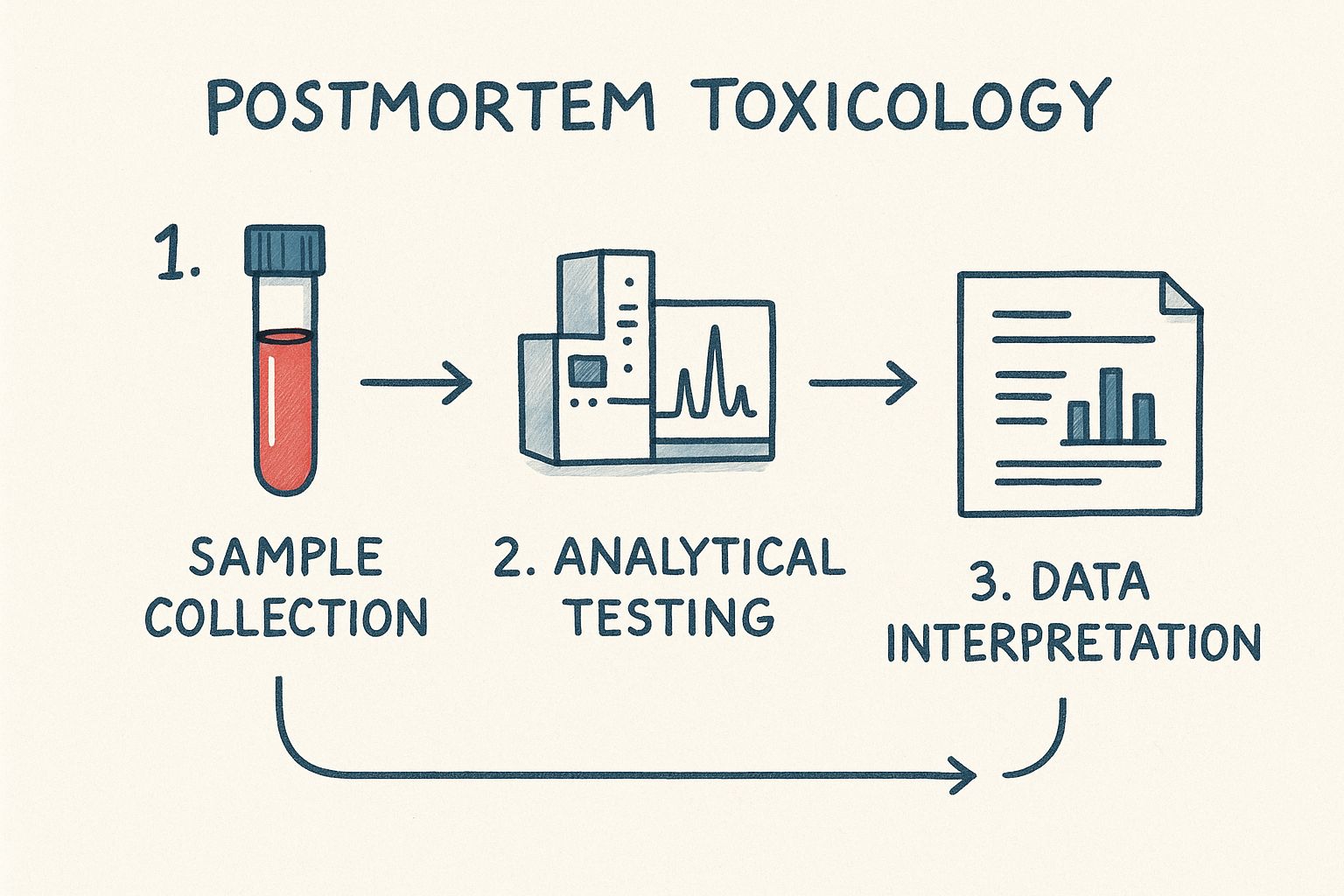
From Autopsy Suite to the Lab
Once collected, samples are meticulously labeled, sealed in tamper-evident containers, and documented to initiate the chain of custody—an unbroken formal record that tracks each specimen from my hands to the laboratory. This procedure is non-negotiable; it guarantees the integrity of the evidence and ensures its legal defensibility.
At the laboratory, analysis typically proceeds in two phases.
The first phase is a broad screening test. Think of this as casting a wide net. These initial tests, often immunoassays, are designed to quickly check for the presence of major drug classes like opioids, benzodiazepines, or amphetamines.
A positive screen is not the end of the story. It is merely the beginning.
The Gold Standard: Confirmation
A positive screening test is an indication, not definitive proof. For that, we move to the second and most critical phase: confirmatory testing.
This is where highly sophisticated technology comes into play. The gold standard is a technique like gas chromatography-mass spectrometry (GC-MS) or its liquid-based counterpart (LC-MS/MS). These instruments separate every component in a sample and identify each one by its unique chemical signature.
Crucially, this provides a quantitative result—the exact concentration of a substance. It’s the difference between a witness saying "the car was speeding" and a radar gun reporting it was going precisely 92 miles per hour. This level of precision is absolutely essential for determining if a substance played a role in the cause of death.
Substances Included in a Toxicology Screen
One of the first questions families often ask is, "What exactly are you looking for?" It’s an excellent question. A postmortem toxicology screen isn’t a single test but a comprehensive investigation designed to capture any substance that could help explain what happened.
To conduct this search methodically, the analysis is broken down into several key categories. This ensures a thorough and efficient process, from well-known street drugs to less obvious household chemicals.
Common Drugs of Abuse
This is the category most people associate with toxicology, and it is a major focus of any toxicology report after death. Testing panels are specifically designed to detect a wide spectrum of substances often linked to impairment, overdose, or accidental death.
This group typically includes:
- Opioids: This is a top priority. We test for everything from heroin and morphine to powerful synthetic opioids like fentanyl and its analogues.
- Stimulants: This includes cocaine (and its metabolite, benzoylecgonine), amphetamines, and methamphetamines.
- Benzodiazepines: These are sedatives like alprazolam (Xanax) or diazepam (Valium). While prescribed legitimately, they are also commonly misused.
- Cannabinoids: This involves testing for THC, the primary psychoactive compound in marijuana.
The devastating opioid crisis has made this work more critical than ever. The role of these substances in overdose deaths highlights why our testing must constantly adapt to the changing landscape of illicit drugs.
Therapeutic and Over-the-Counter Medications
Equally important, but often overlooked, is the role of legal medications. A substance does not have to be illicit to be dangerous. The right medicine at the wrong dose—or mixed with the wrong substance—can be fatal.
We meticulously screen for hundreds of different therapeutic drugs, such as:
- Antidepressants (like SSRIs and tricyclics)
- Antipsychotics
- Cardiac medications (beta-blockers, anticoagulants)
- Pain relievers (acetaminophen, ibuprofen)
- Sleep aids
The presence of a prescribed medication isn’t automatically a red flag. A significant part of my job is interpreting the concentration of the drug found. The goal is to determine if the level is therapeutic (the normal, expected amount), toxic, or potentially lethal.
This distinction is crucial. It helps separate a person who was simply taking their medication as prescribed from a situation involving an accidental or intentional overdose.
Alcohols and Other Volatiles
Alcohol is one of the most common substances we identify. Our analysis focuses on ethanol—the type of alcohol in beer, wine, and spirits. Its presence can be the direct cause of death in cases of acute alcohol poisoning, or it can be a major contributing factor in accidents, falls, and other injuries.
We also look for other "volatile" substances, which are chemicals that vaporize easily and can be inhaled. This category includes:
- Methanol and isopropanol: Toxic alcohols found in products like windshield washer fluid or rubbing alcohol.
- Inhalants: This can include chemicals like difluoroethane, the propellant in compressed air dusters that is sometimes tragically abused.
Special Cases: Poisons and Toxins
Finally, if the circumstances surrounding a death are suspicious or unusual, the search is broadened further. These specialized tests are not routine; they are ordered when something in the case history, at the scene, or during the autopsy points toward a specific type of poisoning.
Some examples of these targeted tests include:
- Carbon Monoxide: Essential for deaths involving fires, faulty heating systems, or vehicle exhaust.
- Cyanide: A rapidly acting poison that requires very specific testing methods for detection.
- Heavy Metals: If poisoning is suspected, we can test for substances like arsenic, lead, or mercury.
By moving through each of these categories, a complete toxicological profile is built. This detailed picture is what gives families clear answers and provides the justice system with the facts it needs.
Making Sense of a Toxicology Report
When you first see a toxicology report, it can be overwhelming. You are faced with a list of scientific terms, chemical names, and numbers that can feel like a foreign language. My role is not only to perform the autopsy but to translate that technical jargon into plain English so you can understand what the findings truly mean.
Interpreting these results is not just about identifying a drug or a number. It is about placing those findings into the context of the individual’s life and the physical autopsy results. This is where a forensic pathologist's experience is crucial—connecting the dots between the laboratory data and what actually happened.
What Was Found vs. How Much Was Found
The first thing to understand is that toxicology results come in two main forms:
Qualitative Results: This is a simple "yes" or "no." It tells us if a substance was present. If a report says a drug was "detected" or "positive," it simply means it was found, even in trace amounts.
Quantitative Results: This is the critical part. It answers the question, "How much of the substance was there?" This is always a number, typically measured in nanograms per milliliter (ng/mL) or milligrams per liter (mg/L). This number provides the context needed to determine if the substance could have caused harm.
Think of it this way: a qualitative result tells you a car was on the road, while a quantitative result tells you if it was traveling 5 mph or 100 mph. For a practical look at how this information is presented, you can review our detailed toxicology report example.
Understanding Concentration Levels
Once we know how much of a substance was present, we must determine what that number means. This is done by comparing it to established reference ranges, which serve as guidelines to help categorize the drug concentration.
It's incredibly important to remember that these ranges are just a starting point. The same concentration of a drug can affect two people very differently depending on their tolerance, age, health, and other individual factors.
To help you make sense of the report, here is a quick guide to the terms you will encounter.
Key Terms in a Toxicology Report
The table below breaks down the common terms used to describe drug concentration levels. Understanding these will help you place the quantitative results into a meaningful context.
| Term | Plain Language Definition | Example Context |
|---|---|---|
| Therapeutic Range | The expected amount of a medication in someone taking it as prescribed. | An individual taking prescribed blood pressure medicine would have a level in this range. |
| Toxic Range | The drug level is high enough to cause serious side effects, impairment, or harm. | A person who accidentally took a double dose of their pain medication might fall into this range. |
| Lethal Range | The concentration is so high that it is often associated with causing death. | A drug overdose will almost always result in a concentration within or above this range. |
Keep in mind that these are guidelines. A long-term drug user might tolerate a "lethal" level, while a novice user could be harmed by a much lower amount.
Why Finding a Drug Doesn't Automatically Mean It's the Cause of Death
This is perhaps the most important concept in postmortem toxicology: the presence of a drug does not automatically mean it caused the death. Interpreting the results is a nuanced process, and several factors can complicate the picture.
Two of the most significant complicating factors are:
Tolerance: An individual who uses a substance regularly—especially opioids or sedatives—develops a tolerance. Their body adapts and can handle blood concentrations that would be fatal to someone without that history.
Postmortem Redistribution (PMR): This is a phenomenon that occurs after death where drugs that have settled into tissues like the liver, lungs, or heart muscle can seep back into the blood, artificially inflating the concentration. This is why blood taken from the heart is often unreliable. The standard of care is to draw blood from a peripheral site, like the femoral vein in the leg, which provides a much more accurate picture of the drug levels at the time of death.
Ultimately, interpreting a toxicology report is an investigative process. The laboratory data must be weighed against the physical autopsy findings, the decedent’s medical history, and the circumstances of their death to form a complete, medically sound conclusion.
Common Misconceptions About Toxicology Reports
Thanks to popular television shows and movies, forensic science has captured the public’s imagination. While this has sparked valuable interest in my field, it has also created many myths about how postmortem toxicology actually works. A significant part of my job is helping families and legal professionals separate Hollywood drama from scientific reality.
Clearing up these misconceptions is the first step toward understanding what a toxicology report after death can—and, just as importantly, cannot—tell us. Let's address some of the most common myths I encounter.
Myth 1: The Results Are Instant
This is perhaps the most pervasive myth. On television, a scientist hands over a complete report within hours. This simply does not happen.
In reality, proper, legally defensible toxicology testing is a slow and painstaking process. Preliminary screening results might be available within a few days, but the detailed, confirmatory testing required for a final report typically takes anywhere from four to twelve weeks. In highly complex cases, it can take even longer. This careful pace is not about delay; it is about ensuring every finding is accurate and can withstand scrutiny in a court of law.
Myth 2: The Presence of a Drug Means It Was an Overdose
It is easy to assume that finding an illicit drug or a high level of a prescription medication automatically means it caused the death. This is a dangerous oversimplification. The presence of a substance is a starting point, not the conclusion.
Context is everything. We must consider the entire picture, including factors such as:
- Tolerance: An individual with a long history of substance use might have levels in their system that would be fatal for a new user but were normal for them.
- Drug Interactions: The cause of death could be a lethal combination of multiple drugs, even if each was at a low or "therapeutic" level on its own.
- Underlying Health: A person with a compromised heart might die from a stimulant dose that a healthy individual could tolerate.
A toxicology report does not exist in a vacuum. It is one critical piece of a much larger puzzle that includes the physical autopsy, medical history, and scene evidence. Only by integrating all of these components can we arrive at the truth.
Myth 3: A Negative Report Means No Substances Were Involved
If a report comes back "negative," it seems logical to conclude that no drugs or toxins were involved. However, that is not always the case. A standard toxicology panel is designed to detect the most common substances—it cannot test for every single compound in existence.
The world of synthetic drugs is constantly evolving, with new substances that may not appear on a routine screen. Furthermore, some drugs are metabolized and eliminated from the body so quickly that they become undetectable soon after death. A negative report simply means nothing was found within the scope of the specific tests that were performed.
This is a moving target that varies globally. For instance, regional drug-related death trends in Europe show shifting patterns, with some countries seeing more fatalities from synthetic cannabinoids while others deal with different emerging threats. These differences illustrate why an investigation must remain flexible and consider all possibilities, even when initial tests are negative.
Next Steps After Receiving the Report
Receiving the final autopsy and toxicology reports can feel like the end of a long and difficult wait. In reality, it marks the beginning of the next phase—one where all the scientific data is synthesized to provide answers and inform necessary actions.
The toxicology report after death is never a standalone document. As a forensic pathologist, my responsibility is to integrate these results with the physical findings from the autopsy, the decedent's medical history, and information from the scene investigation. This holistic approach allows me to finalize the death certificate with a conclusion that is both medically accurate and legally sound.
Scheduling a Conference to Review Findings
For families, the most important next step is to schedule a meeting with the forensic pathologist who performed the autopsy. I cannot stress this enough. This is a private, dedicated time for us to review the report line by line and for me to answer every question in a compassionate, unhurried manner.
This meeting is your opportunity to gain the clarity you deserve. We can cover topics such as:
- Explaining technical terms: I will translate complex medical language into plain, understandable English.
- The impact of substances on the body: We will discuss the role each detected drug or chemical played, if any.
- The final cause and manner of death: I will explain how all the evidence led to the final conclusion.
This conversation is often a significant step toward finding closure. It helps replace uncertainty and speculation with a factual understanding of what occurred, which is a powerful part of the grieving process. Our guide on how long autopsy results take can provide a better sense of the overall timeline.
The Report's Role in Legal Matters
For attorneys and legal professionals, these finalized reports are the bedrock of a case. They serve as critical, objective evidence in both civil and criminal proceedings, cutting through speculation with unbiased scientific data.
In a wrongful death lawsuit, for instance, a toxicology report could be the key piece of evidence that links a death to an act of negligence, such as a medication error or exposure to a workplace toxin. The scientific objectivity of the report makes the case compelling.
These documents provide the factual basis needed to pursue justice, establish liability, and ensure legal outcomes are built on sound science. My team and I are available for professional consultation for attorneys with questions about a complex report.
Answering Your Questions About Toxicology Reports
When you are coping with the loss of a loved one, you are bound to have many questions. From my experience, the toxicology report is often one of the most confusing aspects of the postmortem process. Allow me to address some of the most common questions I hear from families and legal professionals to provide some clarity.
How Long Does a Toxicology Report Take to Complete?
This is the most frequent question I receive, and the honest answer is: it takes time. While the physical autopsy is typically completed within a day or two, the laboratory work is a much more deliberate process.
Initial screening results may be available in a few days, but the full, legally defensible report takes much longer. You can generally expect it to take between four to eight weeks. For very complex cases involving new or unusual substances, it could extend for several months. I understand the wait is difficult, but this time is essential to ensure complete scientific certainty.
Can a Family Request Specific Drug Testing?
Yes, absolutely. In fact, your input is incredibly helpful. If you have knowledge of your loved one’s medical history, prescriptions, or have concerns about a specific substance, please share that information.
While I always run a comprehensive set of standard tests based on the case circumstances, a family's insight can help focus the investigation and ensure nothing is overlooked. Though the final decision on which tests to run rests with the pathologist, I take every family request very seriously as we work together to be as thorough as possible.
What Happens if a Report Is Inconclusive?
It is rare, but a report can sometimes be inconclusive. This might happen if the samples were degraded, a novel synthetic drug was involved that our tests cannot yet identify, or a substance level was in a gray area between therapeutic and toxic.
In such cases, the toxicology report is just one piece of a much larger puzzle. The cause of death must be determined by evaluating all other available evidence.
We will integrate all other information: the findings from the physical autopsy, the decedent’s complete medical history, and evidence from the scene investigation. If a definitive cause still cannot be pinpointed after considering all the evidence, the cause of death may be ruled "undetermined."
At Texas Autopsy Services, we understand the importance of clear, compassionate answers during a difficult time. If you have questions about private autopsy services or need assistance interpreting complex medical findings, our team is here to provide the support you need. Please do not hesitate to contact us by phone or email for a confidential conversation about your situation.
Learn more at https://www.texasautopsyservices.com.