Forensic pathology is a specialized field of medicine that provides answers when a death is sudden, violent, or unexplained. At its core, my work is to determine the cause and manner of death. As a forensic pathologist, I am a medical doctor who performs autopsies and investigates the circumstances surrounding a person's passing to give clear, evidence-based answers to families and the legal system. This discipline demands precision, compassion, and a deep-seated commitment to uncovering the truth.
This work is, in many ways, a final act of patient care.
- Forensic pathology uses medical science to determine why a person died.
- The primary goals are to establish the cause of death (the specific injury or disease) and the manner of death (natural, accident, suicide, homicide, or undetermined).
- It serves families by providing closure, public health by identifying trends, and the justice system with objective facts.
- This field requires extensive training, including medical school, a pathology residency, and a specialized forensic pathology fellowship.
Defining Forensic Pathology: A Search for Answers
When someone passes away under tragic or unclear circumstances, they leave behind a void filled with difficult questions. My role as a forensic pathologist is to step into that space and methodically find answers. The reality of this work is far from the fast-paced drama often depicted on television; it is a quiet, careful, and deeply scientific process.
Ultimately, forensic pathology is a final act of patient care. We are physicians first, using our expertise in disease and injury to explain precisely why a person died. This work provides closure for grieving families, critical data for public health, and objective facts for the justice system.
The Core Responsibilities
At its heart, my profession is about bringing clarity to complex situations. We apply rigorous medical science to death investigation, ensuring every conclusion is built on solid evidence. The role is a blend of medical knowledge and diligent investigation.
In every case, my primary objective is to serve the truth. Each examination is conducted with profound respect for the decedent, understanding that our findings provide a crucial voice for those who can no longer speak for themselves.
The work extends far beyond the autopsy itself. We review medical records, analyze the circumstances surrounding the death, and conduct detailed examinations to reconstruct the final moments of a person's life. It is this comprehensive approach that ensures our findings are accurate and reliable.
Here is a breakdown of the primary duties that define the work of a forensic pathologist. Each is a crucial piece of a puzzle that, when assembled, reveals a clear and defensible medical story.
Core Responsibilities of a Forensic Pathologist
| Responsibility | Description | Example |
|---|---|---|
| Determine Cause of Death | Identifying the specific disease or injury that directly initiated the process of death. | A gunshot wound to the chest, a myocardial infarction (heart attack), or complications from influenza. |
| Determine Manner of Death | Classifying the death into one of five categories based on the circumstances. | Categorizing a death as natural, accident, suicide, homicide, or undetermined. |
| Document Findings | Creating a detailed, objective report of all observations and laboratory results. | The final autopsy report, which becomes a vital legal and medical document. |
| Testify in Court | Providing expert medical testimony to explain complex findings to a judge and jury. | Clearly explaining the physiological effects of a specific injury during a homicide trial. |
Each responsibility is interconnected, forming a comprehensive process that ensures every death is properly understood and documented for the family, for public record, and for the law.
Tracing the Scientific Roots of Forensic Pathology
The principles guiding modern forensic pathology are not new; they are the product of a centuries-long search for medical truth. Long before our field had a name, physicians and scientists sought to understand death not as an unexplainable event, but as a biological process that could be carefully studied.
This journey—from simple observation to a rigorous, methodical science—is what gives our work its authority today. Our practice is built on a foundational idea: the human body holds its own story, and with the right methods, we can learn to read it.
The Father of Modern Pathology
The field took a monumental leap forward in the 19th century thanks to a German physician named Rudolf Virchow. His contributions were so fundamental that he is widely known as the "father of modern pathology." Virchow championed the then-revolutionary idea that diseases originate at the cellular level, which completely transformed how doctors viewed the body.
He brought that same microscopic, detail-oriented focus to the study of death. Before Virchow, autopsies were often limited, perhaps only examining an obvious wound or a single diseased organ. Virchow insisted on a far more comprehensive approach.
At its core, forensic pathology is built on a systematic foundation. It's the belief that by examining the whole, we can understand the sum of its parts and how their failure led to a final, irreversible outcome. This comprehensive view is a direct legacy of Virchow's work.
Establishing a Scientific Standard
This meticulous process became known as the Virchow method. It is a systematic technique involving a head-to-toe examination of the entire body, turning the autopsy from a cursory look into a standardized, scientific procedure. This method remains one of the principal techniques used today, and it is the best way to ensure no detail is overlooked. You can delve deeper into these foundational techniques by exploring the origins of forensic pathology.
Having this framework allows us to build a complete picture. It ensures every examination is consistent and thorough—qualities that are absolutely critical when findings may be presented in a courtroom or provide long-awaited answers for a family.
From Past to Present Practice
The spirit of Virchow’s work is very much alive in what we do today. While our tools have advanced significantly—from high-resolution imaging to genetic analysis—the core principle remains unchanged: every investigation must be thorough, objective, and grounded in solid medical science.
The history of forensic pathology is a powerful reminder that our search for answers stands on the shoulders of giants. They established the standards we uphold, and we honor that legacy by bringing the same scientific diligence to every single case. This deep-rooted history is why the field is so trusted—it is a discipline tested and refined through generations of dedicated practice, always in the service of truth.
What a Forensic Pathologist Actually Does in an Investigation
When people learn what I do, their minds often jump straight to the autopsy suite. And while the postmortem examination is a central component of my work, it is just one piece of a much larger investigative puzzle. My work as a forensic pathologist often begins long before the first incision and continues well after I have signed the final report.
An investigation can be thought of as a careful reconstruction of a person’s final hours, days, or even weeks. It all starts not with a scalpel, but with information. We review medical histories, confer with law enforcement about the circumstances of the death, and piece together the context. This groundwork is absolutely essential.
Sometimes, this includes visiting the scene of the death. Being physically present can reveal subtle clues that would otherwise be missed—details that help connect what we find during the examination to the environment where a life ended. It is all about gathering every possible thread before the physical examination begins.
Cause and Manner of Death: The Two Pillars of a Forensic Report
To understand the core of my job, it is crucial to grasp the difference between two critical concepts: the cause of death and the manner of death. They may sound similar, but they answer completely different questions and carry significant legal and personal implications.
Cause of Death: This is the specific medical reason a person is no longer alive—the injury or disease that initiated the chain of events leading to death. It is the purely biological answer to the question, "What happened?"
Manner of Death: This is a legal classification based on all available information, including the cause of death and the circumstances surrounding it. It answers the question, "How did it happen?"
It is this second determination—the manner of death—where the initial investigative work truly proves its value. It is not just a medical conclusion; it is a judgment based on the totality of the evidence.
I often explain it this way: The cause of death is the destination—the medical event that ended the journey. The manner of death is the vehicle that led there. Was it a natural event, an accident, or something else?
The Five Manners of Death
In the United States, every death certificate includes one of five classifications for the manner of death. This classification is incredibly important for families, for insurance purposes, and for the justice system.
- Natural: Death caused solely by disease or the natural aging process. This is the most common manner of death.
- Accident: An unplanned, unintentional event that results in death, such as a motor vehicle collision, a fall, or an accidental drug overdose.
- Suicide: A death that results from a person's own intentional, self-inflicted act.
- Homicide: A death that occurs at the hands of another person. This is a medical determination, not a legal one; it does not automatically mean "murder."
- Undetermined: This classification is used when there is insufficient evidence to confidently place the death into one of the other four categories.
Each case is a profound responsibility. The final report must be a clear, objective document built on a foundation of solid fact. It becomes the last medical record for that individual and a source of truth for their family. The extensive, specialized training required for this work is something you can learn more about by exploring the background of the doctors that do autopsies.
Ultimately, our role is to be a voice for the deceased. We translate complex medical findings into clear, understandable facts so that families can find closure and the justice system can act on accurate information. It is a duty I take very seriously in every single investigation.
The Autopsy: A Respectful Medical Examination
The word "autopsy" can be unsettling. For many families, it brings to mind dramatic scenes from movies or television. As a forensic pathologist, I want to demystify this process and show you what it truly is: a thorough, respectful medical examination aimed at one thing—finding answers.
Every step is performed with the utmost care and precision. This is not a macabre procedure; it is the final act of medical care, dedicated to uncovering the truth with dignity.
The External Examination
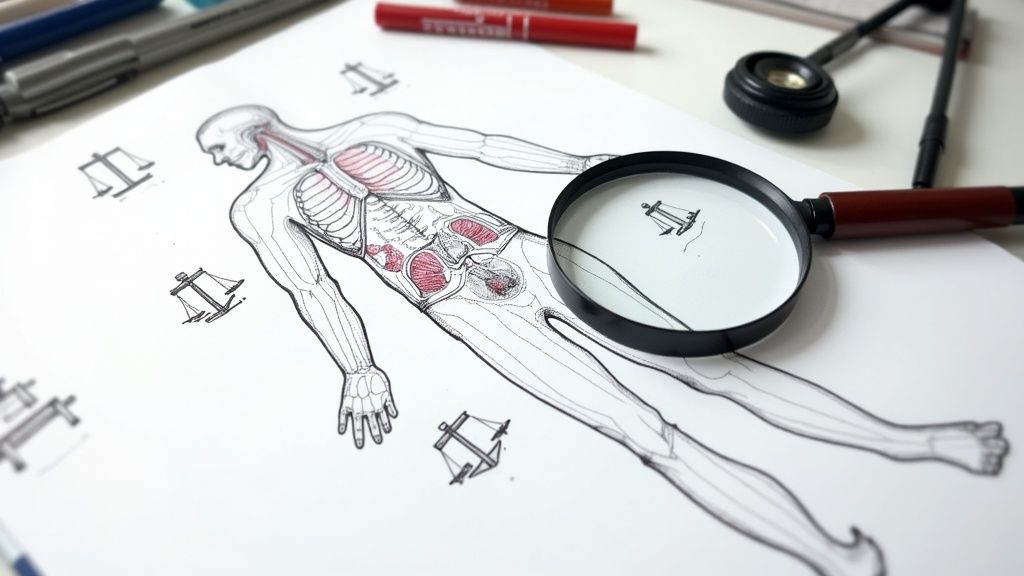
We always begin with an external examination. Long before any internal analysis, I conduct a comprehensive, head-to-toe inspection of the body. This is a critical information-gathering phase that tells us a great deal about the person and the circumstances surrounding their death.
During this stage, I document everything in minute detail:
- Identifying Features: Scars, tattoos, and other unique marks help confirm the individual's identity.
- Evidence of Injury: I carefully note any bruises, abrasions, wounds, or other signs of trauma. Each finding's size, shape, and location is precisely measured and recorded.
- Signs of Medical Intervention: The presence of surgical scars, intravenous lines, or other medical devices can provide clues to a person's recent health history.
This initial, non-invasive step lays the groundwork for the entire examination. It is all about observation and documentation, building the first pieces of the case's framework.
The Internal Examination
After the external review is complete, we proceed to the internal examination. This is where we can directly observe the organs to identify disease or injury that was not visible from the outside. The entire process is systematic to ensure nothing is missed.
Each organ is carefully examined, weighed, and measured. We take small tissue samples—often no larger than a postage stamp—for microscopic analysis. This specialized field, known as histology, allows us to see signs of disease at the cellular level. It can reveal conditions like infections, heart disease, or cancer that might have contributed to the person's death.
This graphic provides a clear overview of the methodical, three-step process we follow in most postmortem examinations.
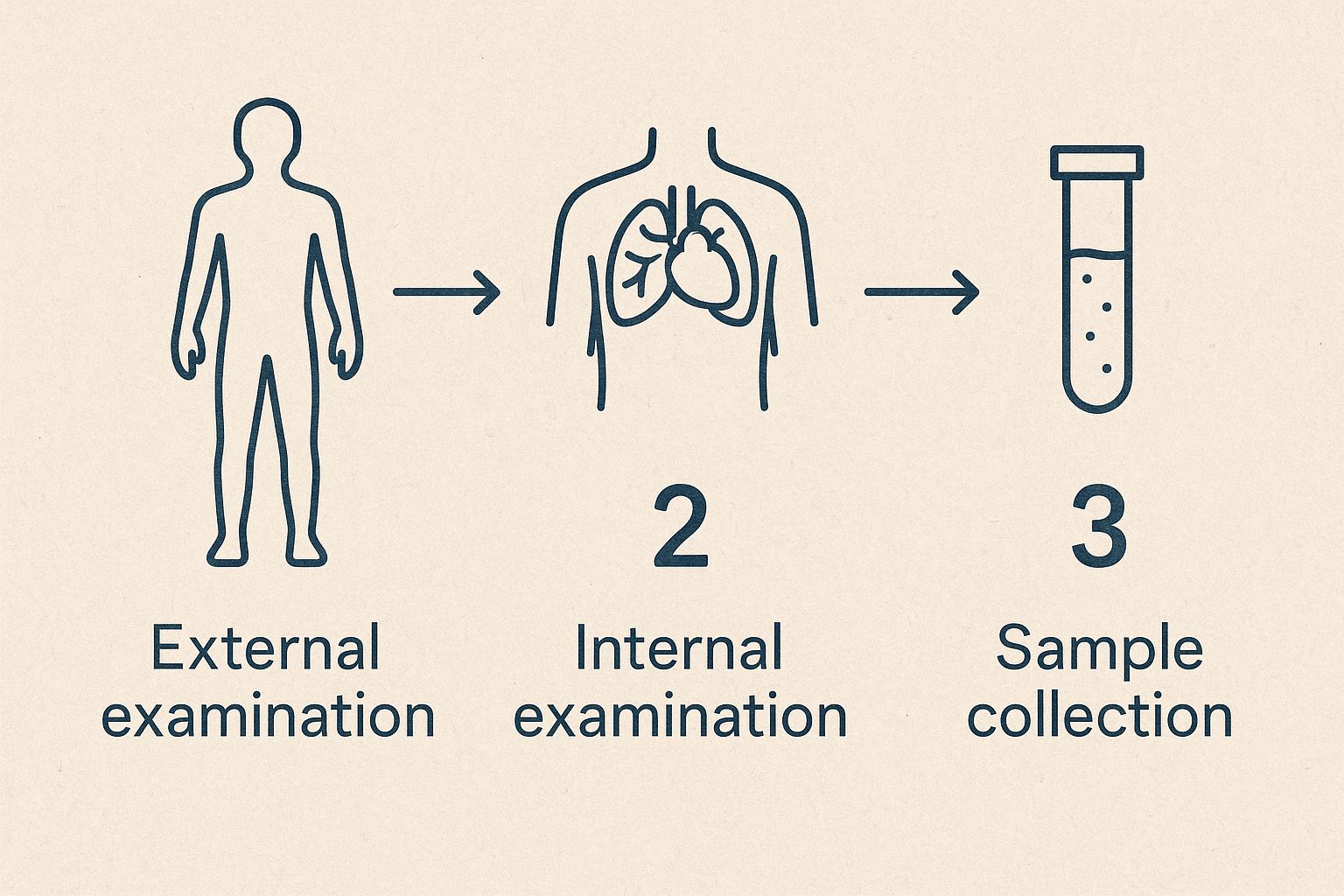
As you can see, an autopsy is a highly structured medical procedure, moving logically from external observation to internal analysis and, finally, to specialized laboratory tests.
Sample Collection for Further Studies
The last part of the hands-on examination involves collecting fluid and tissue samples for additional laboratory testing. These ancillary studies are often essential for completing the full diagnostic picture.
Toxicology, for example, is the analysis of blood and other bodily fluids to check for the presence of alcohol, prescription medications, illicit drugs, or poisons. These results can be absolutely critical in determining the cause of death, especially if an overdose or poisoning is suspected. During this process, we also review the decedent's medical history, which often means understanding medical classification systems like ICD-10 to ensure our findings are documented accurately.
The need for medical expertise in death investigation has long been recognized. In fact, Maryland passed a pioneering law back in 1860 requiring a trained physician to be present at all death inquests. It was a landmark move that helped establish medical fact, not just speculation, as the foundation of these investigations.
Each sample collected, each measurement taken, and each observation noted is a piece of a larger puzzle. My job is to assemble these pieces into a coherent, factual narrative that honors the deceased and provides clarity for their loved ones.
It is important to remember that not every death investigation requires a full autopsy. That decision is made carefully, based on the specific questions that need answers. You can learn more about when autopsies are performed in our detailed guide. Ultimately, the autopsy is a powerful tool we use to provide definitive, medically sound answers when they are needed most.
The Tools of the Trade: Modern Forensic Techniques
An autopsy provides a massive amount of information, but it rarely tells the whole story on its own. What we observe with our eyes is just the beginning. The real power of a modern forensic investigation comes from looking deeper with advanced scientific testing.
Think of the autopsy as the command center for the investigation. From here, we send tissue and fluid samples for various specialized analyses. Each test result returns like a puzzle piece, helping us build a complete, defensible picture of what happened.
Beyond the Naked Eye: Essential Lab Tests
Two of the most critical tools in our arsenal are toxicology and histology. These studies are routine in many of my examinations because they answer questions that a physical inspection simply cannot. They provide the microscopic and chemical story of a person's final moments.
- Toxicology: This is the science of detecting and measuring drugs, alcohol, poisons, or other chemicals in the body. By testing blood, urine, or tissue, we can determine not just if a substance was present, but also how much. This is key to determining if a dose was therapeutic, toxic, or lethal, which is vital in suspected overdose or poisoning cases.
- Histology: This is the examination of tissue under a microscope. By preparing incredibly thin slices of organs and staining them, we can identify diseases and injuries at the cellular level. This might reveal a hidden heart condition that caused a sudden collapse, an infection that went unnoticed, or microscopic internal damage that was otherwise invisible.
These tests elevate an investigation from a set of observations to a full scientific analysis. They provide the objective data needed to connect the circumstances of the death to the physical evidence found during the autopsy.
It Takes a Team: The Collaborative Effort of Forensics
A forensic pathologist never works in a vacuum. A thorough medicolegal investigation is a true team effort, blending our medical findings with evidence from many other forensic experts. This collaboration is what makes modern forensic science so powerful and reliable.
We are in constant communication with other specialists to ensure all the evidence aligns.
For example:
- DNA analysts can help identify an unknown person or link an individual to a scene.
- Ballistics experts can match a bullet I recover during an autopsy to the specific firearm that discharged it.
- Fingerprint specialists can provide evidence about who was—or was not—at a key location.
This team-based approach has a long history. As far back as 1811, the French investigator Eugene Vidocq created one of the first organized detective units, using then-new methods like ballistics and footprint analysis to solve crimes. His work began a tradition of scientific collaboration that we continue today. If you're curious, you can explore more about the fascinating history of forensics.
By weaving together these different threads of evidence, we ensure our final opinion on the cause and manner of death is not just a medical judgment, but a conclusion backed by a solid, complete body of scientific fact.
The Journey to Becoming a Forensic Pathologist
Becoming a forensic pathologist is a marathon, not a sprint. It is a path that demands more than a decade of intense, specialized training, and it is a commitment few are prepared to undertake. This journey is deliberately rigorous, designed to produce physicians who can investigate death with absolute scientific accuracy.
This extensive education is precisely why families and the legal system can place their trust in our findings. Every single step builds on the last, culminating in a level of expertise that simply cannot be fast-tracked.
The Educational Pathway
The training is structured and non-negotiable, ensuring every certified practitioner meets an exceptionally high standard. It is a long road, but each stage is critical for developing the skills needed to untangle the complexities of a medicolegal death investigation.
Here is what that journey looks like:
- Undergraduate Degree: A four-year bachelor's degree, typically with a strong emphasis on pre-medical sciences like biology and chemistry.
- Medical School: Four years of intensive medical education to earn a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree.
- Pathology Residency: A three to four-year residency where physicians learn to diagnose diseases by examining tissues and bodily fluids. This is the foundation of all pathology.
- Forensic Pathology Fellowship: The final step is a one-year, highly specialized fellowship focused entirely on the practice of medicolegal death investigation. This is where a pathologist learns to connect medical findings to a legal context.
Only after completing this 12 to 13-year journey can a doctor sit for their board examinations to become a certified forensic pathologist. For a more detailed breakdown, we’ve put together a complete roadmap in our guide on how to become a forensic pathologist.
Essential Qualities Beyond the Diplomas
While the academic and clinical training is exhaustive, certain personal qualities truly define an excellent forensic pathologist. The work requires a unique blend of intellectual rigor and profound emotional strength.
Technical skill alone is not enough. This profession demands an unshakeable ethical compass and the ability to remain objective and compassionate, often in the face of unimaginable tragedy. It is a constant balance between clinical detachment and human empathy.
Certain traits are simply non-negotiable:
- Meticulous Attention to Detail: The smallest observation—a subtle bruise, a microscopic fiber—could be the key to unlocking an entire case.
- Emotional Resilience: One must be able to confront tragic and often disturbing circumstances daily without losing focus or humanity.
- Unwavering Objectivity: Findings must be based purely on the evidence, free from emotion or outside pressure.
This combination of deep training and innate personal traits ensures that when a forensic pathologist presents their findings, they speak with the full authority of medical science and ethical integrity.
Frequently Asked Questions About Forensic Pathology
Families often come to me with many of the same questions. When you are navigating the loss of a loved one, it is natural to want clear answers about the process, and I believe you deserve them. Let's walk through some of the most common things people ask about my work.
What's the Difference Between a Coroner and a Medical Examiner?
This is perhaps the most common point of confusion, and it is a significant one. While the roles may sound similar, the training and qualifications behind them can be worlds apart.
A medical examiner is a physician—specifically, a forensic pathologist like me—who is appointed to their role. We are doctors who have specialized in death investigation. In contrast, a coroner is often an elected official who may not have any medical background. Because of this distinction, many jurisdictions, including large areas of Texas, have transitioned to a medical examiner system to ensure that a medical expert leads these critical investigations.
Is an Autopsy Always Required in a Forensic Case?
No, not at all. An autopsy is a powerful diagnostic tool, but it is one we use only when necessary. If the cause and manner of death are clear from an examination of the scene, the body, and the known circumstances, a full internal examination may not be required.
For instance, in a witnessed motor vehicle collision with obviously fatal injuries, a full autopsy might not yield additional crucial information for the death certificate. We make that determination on a case-by-case basis, guided by legal requirements and what is needed to establish the facts.
Private Autopsy vs. County Autopsy: What's the Difference?
This distinction comes down to who initiates the process and why. A county or state medical examiner performs an autopsy because the law requires it for public health and legal reasons—such as in sudden, suspicious, or violent deaths.
A private autopsy is different. It is a service requested directly by a family. This often occurs when a death does not legally require a government-mandated autopsy, but the family still has unanswered questions. Perhaps they have concerns about the medical treatment their loved one received or wish to know if a genetic condition played a role. A private autopsy serves the family's need for answers, first and foremost.
How Does Forensic Pathology Help Public Health?
We often serve as the first line of defense in identifying hidden threats to community health. By determining precisely why people have died, we can uncover patterns that might otherwise go unnoticed.
For instance, if we begin to see a cluster of deaths from an unusual infection, we can alert public health officials to a potential outbreak. Our findings on drug overdoses, carbon monoxide poisonings from faulty heaters, or defects in consumer products all contribute data that drives safety recalls and public awareness campaigns. It is work that quietly saves lives.
If you are left with unanswered questions after a loss, our team at Texas Autopsy Services is here to help you find clarity. Please feel free to contact us by phone or email to see how an independent autopsy can provide the answers you need.